Co-Infection with Nocardia and Mycobacterium Avium Complex (MAC) in a Patient with Acquired Immunodeficiency Syndrome
 Thursday, January 24, 2019 at 8:00AM
Thursday, January 24, 2019 at 8:00AM Zahira Babwani DO
Kenneth Wojnowski Jr DO
Sunil Kumar MD
Broward Health Medical Center
Fort Lauderdale, FL USA
Abstract
We present a case in which a patient with acquired immunodeficiency syndrome (AIDS) and nocardiosis was found to have co-infection with Mycobacterium avium complex (MAC). Despite the fact that MAC is a known colonizer of the pulmonary system, it is possible to have co-infection and a high degree of suspicion is necessary to ensure prompt treatment of both organisms. We wish to describe how radiologic findings were instrumental in guiding our differential diagnosis.
Case Report
History of Present Illness: A 64-year-old man with history of alcohol and tobacco abuse presented with a chronic, productive cough for 5-6 months. Associated symptoms included shortness of breath and 30-pound weight loss. He denied all other symptoms.
Physical Exam: Pertinent positives revealed temporal wasting, poor dental hygiene, oral thrush and diffuse rhonchi bilaterally. Initial vital signs were within normal limits.
Laboratory and Radiology: Pertinent laboratory findings revealed leukocytosis with a left shift. Viral respiratory polymerase chain reaction (PCR) testing was negative. Human immunodeficiency virus (HIV) testing was positive with a CD4 count of 46 cells/mm3. QuantiFERON gold testing was negative. Sputum cultures, acid-fast bacilli (AFB) and blood cultures were obtained. Bronchoalveolar lavage (BAL) was performed with no evidence of Pneumocystis jirovecii (PJP). Chest X-ray (CXR) and computed tomography (CT) of the chest (Figure 1) revealed a multifocal right lung abscess with complex pleural fluid, empyema, nodular cavitary lesion in the left lower lobe and hilar lymphadenopathy.
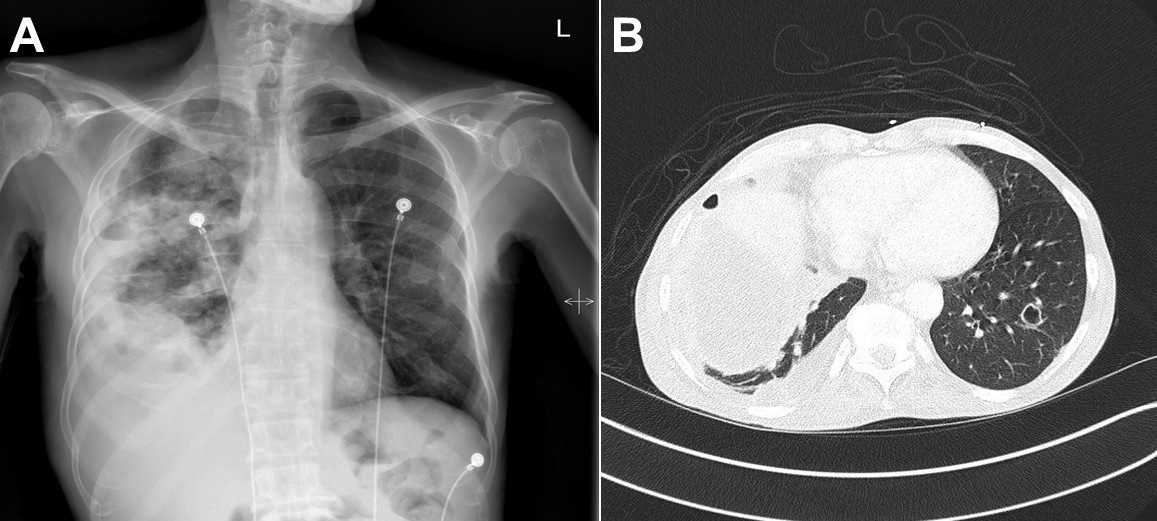
Figure 1. Panel A: initial chest X-ray shows a complex infiltrate and effusion in the right lung. There is a cavitary lesion with air-fluid level vs lung abscess on the right. A nodule or consolidation is present in the left lung base. Panel B: A representative image from the initial CT of the chest showing a multifocal right lung abscess and complex pleural fluid.
Hospital Course: After admission, the patient was started on broad spectrum antimicrobials with vancomycin and piperacillin-tazobactam. A thoracentesis was performed due to right sided pleural effusion which yielded 65 cc of thick, purulent, green fluid. Thoracotomy with complete decortication of the right lung was performed with biopsies of the abscesses. Two 32-French chest tubes were placed due to the presence of multiple intraparenchymal lung abscesses, loculations, and empyema. Biopsy and pleural fluid cultures grew gram positive, beaded organisms which were later identified as nocardia, with no evidence of MAC or Mycobacterium tuberculosis (MTB). The patient was started on amikacin, meropenem and trimethoprim-sulfamethoxazole for newly diagnosed pulmonary nocardiosis. MAC prophylaxis was initiated due to his low CD4 count. After initiation of therapy for nocardiosis, three sputum AFB cultures began to stain positive. Since nocardiosis stains weakly positive for AFB, we initially did not suspect non-tuberculous Mycobacteria (NTM). Repeat CT scan of the chest (Figure 2) revealed ground glass opacities, nodular densities and both mediastinal and hilar lymphadenopathy.

Figure 2. Panel A: after initiation of treatment for nocardiosis, improvement of right empyema and cavitary lesion with bilateral patchy airspace disease right greater than left. Panel B: CT of the chest after initiation of treatment for nocardiosis, prominent lymph nodes in the hilar regions and mediastinum. less cavitation than the previous study. There are innumerable ground glass and nodular densities throughout both lungs, right greater than left.
Suspicion for active MAC co-infection was raised, the prophylactic dose of azithromycin was increased to the treatment dose, and ethambutol was initiated. After three weeks of intravenous amikacin, meropenem and trimethoprim-sulfamethoxazole the patient showed considerable improvement in his respiratory symptoms and was transitioned to oral trimethoprim-sulfamethoxazole for outpatient treatment of nocardiosis with continuation of ethambutol and clarithromycin for MAC.
Discussion
The Mycobacterium Avium Complex (MAC) is a Non-tuberculous mycobacterium (NTM) that is commonly found in patients with HIV and a CD4 count of less than 50. The diagnosis of NTM is challenging due to the fact that the organism is a known colonizer of the pulmonary system (1) . Supportive radiologic evidence is needed to distinguish colonization from active infection (2).
Common CT findings of nocardiosis include ground glass opacities, lung nodules, cavitation, pleural effusion and masses (3). The presence of mediastinal and hilar lymphadenopathy is the most common finding in immunosuppressed patients with MAC infection but is not a usual feature of pulmonary nocardiosis (3,4) . Our patient’s repeat CT scan showed mediastinal and hilar lymphadenopathy with improvement of cavitary lesions which suggests improvement of CT findings related to nocardiosis, but persistent findings related to NTM (5). This led us to believe that the patient was appropriately treated for nocardiosis, but with an underlying presence of active MAC infection that presented with atypical radiographic findings. As per the American Thoracic Society (ATS) guidelines for NTM pulmonary infection (6) , this patient’s pulmonary symptoms, radiological evidence on the chest CT, and positive AFB cultures from at least two separate expectorated sputum samples lends credibility to MAC as a true active infection in the setting of nocardiosis and AIDS. The patient was appropriately placed on clarithromycin and ethambutol as an outpatient, and our suspicions were confirmed for MAC with no evidence of MTB by PCR testing 5 weeks after initial AFB smears were collected.
Co-infection with Nocardiosis and MAC may be underestimated since they both often develop in immunocompromised hosts. MAC, along with other NTM species account for 20% of mycobacterium pulmonary infections in HIV infected patients (5). Nocardia accounts for less than 3% of pulmonary infections in HIV infected patients (5). A high degree of clinical suspicion is imperative to promptly treat infection with both organisms.
References
- Young J, Balagopal A, Reddy NS, Schlesinger LS. Differentiating colonization from infection can be difficult Nontuberculous mycobacterial infections: Diagnosis and treatment. Patient Care. 2007. Available at: http://www.patientcareonline.com/infection/differentiating-colonization-infection-can-be-difficult-nontuberculous-mycobacterial-infections (accessed 10/3/18).
- Trinidad JM, Teira R, Zubero S, Santamaría JM.Coinfection by Nocardia asteroides and Mycobacterium avium- intracellulare in a patient with AIDS. Enferm Infecc Microbiol Clin. 1992 Dec;10(10):630-1. [PubMed]
- Kanne JP, Yandow DR, Mohammed TL, Meyer CA. CT findings of pulmonary nocardiosis. AJR Am J Roentgenol. 2011 Aug;197(2):W266-72. [CrossRef] [PubMed]
- Erasmus JJ, McAdams HP, Farrell MA, Patz EF Jr. Pulmonary nontuberculous mycobacterial infection: radiologic manifestations. Radiographics. 1999 Nov-Dec;19(6):1487-505. [PubMed]
- Benito N, Moreno A, Miro JM, Torres A. Pulmonary infections in HIV-infected patients: an update in the 21st century. Eur Respir J. 2012 Mar;39(3):730-45. [CrossRef] [PubMed]
- Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007 Feb 15;175(4):367-416. [CrossRef] [PubMed]
Cite as: Babwani Z, Wojnowski K Jr, Kumar S. Co-Infection with Nocardia and Mycobacterium avium complex (MAC) in a patient with acquired immunodeficiency syndrome. Southwest J Pulm Crit Care. 2019;18(1):22-5. doi: https://doi.org/10.13175/swjpcc123-18 PDF

Reader Comments