August 2018 Imaging Case of the Month: Dyspnea in a 55-Year-Old Smoker
 Monday, August 6, 2018 at 8:00AM
Monday, August 6, 2018 at 8:00AM Michael B. Gotway, MD
Department of Radiology
Mayo Clinic Arizona
Scottsdale, AZ USA
Clinical History: A 55–year old woman presented to the emergency room with complaints of shortness of breath and lower extremity swelling. The patient noted her shortness of breath had been worsening over the previous 6 months, especially in the last 3 months. The patient denies cough, fever, chills, and night sweats. The patient admits to some fatigue but has not lost weight recently.
The patient is a current smoker, averaging about 1 pack-per-day for the previous 40 years. Her allergies include penicillin and sulfa drugs, and her prior medical history was remarkable only for hypothyroidism and gastroesophageal reflux. Her only previous surgery was for an ectopic pregnancy. The patient’s mediation list included use of opiates for pain related to a herniated disc in the lower cervical spine following an automobile accident two years earlier.
Her physical examination was unremarkable aside from obesity and mild symmetric lower extremity edema. Her vital signs were within normal limits.
Frontal and lateral chest radiography (Figure 1) was performed.
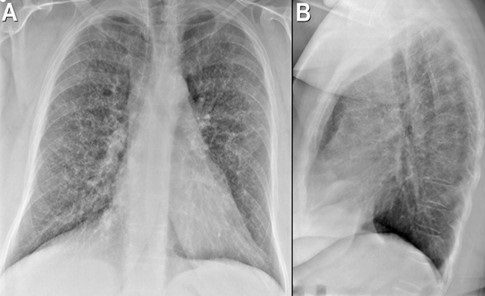
Figure 1. Frontal (A) and lateral (B) chest radiography.
Which of the following represents the most accurate assessment of the chest radiographic findings? (Click on the correct answer to be directed to the second of ten pages)
- Chest radiography shows a mediastinal mass
- Chest radiography shows cavitary pulmonary lesions
- Chest radiography shows miliary nodules
- Chest radiography shows an interstitial abnormality consisting of reticular and nodular opacities
- Chest radiography shows basilar fibrotic opacities
Cite as: Gotway MB. August 2018 imaging case of the month: Dyspnea in a 55-year-old smoker. Southwest J Pulm Crit Care. 2018;17(2):59-69. doi: https://doi.org/10.13175/swjpcc099-18 PDF

Reader Comments