August 2017 Imaging Case of the Month
 Thursday, August 3, 2017 at 8:00AM
Thursday, August 3, 2017 at 8:00AM Brandon T. Larsen, MD, PhD1
Michael B. Gotway, MD2
Departments of Pathology1 and Radiology2
Mayo Clinic Arizona
Scottsdale, Arizona USA
Clinical History: A 67-year-old man with a 23 pack-year history of smoking, stopping 6 years earlier, presented with a year-long history of intermittent hemoptysis consisting of small specs of blood particularly in the morning after he awoke. No sputum discoloration was reported and the patient denied shortness of breath, fever, shortness of breath, and chills. The patient also denied rash, joint pain, and night sweats. His past surgical history was remarkable only for an appendectomy, tonsillectomy, and repair of an ankle fracture, all as a young man. The patient did report some asbestos exposure in the past. He takes a multivitamin and occasional over-the counter pain relievers, but was not taking prescription medications.
Physical examination: unremarkable and the patient’s oxygen saturation was 98% on room air.
Laboratory evaluation: largely unremarkable. Quantiferon testing for Mycobacterium tuberculosis was negative. An outside otolaryngology examination was reported to show no abnormalities. Frontal chest radiography (Figure 1) was performed.
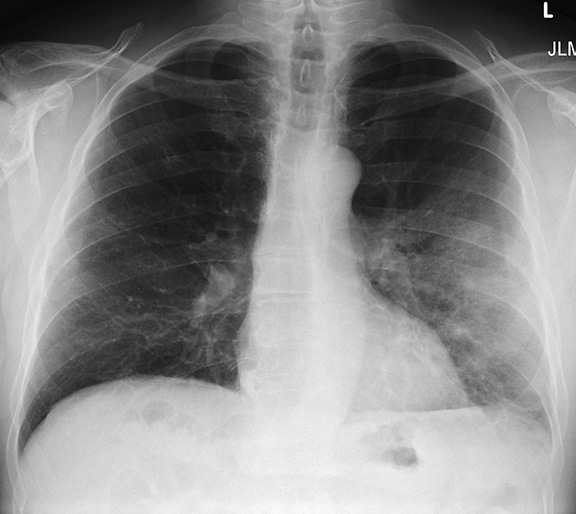
Figure 1. Frontal chest radiography.
Which of the following statements regarding the chest radiograph is most accurate? (Click on the correct answer to proceed to the second of nine pages)
- The chest radiograph shows a mediastinal mass
- The chest radiograph shows multifocal consolidation and pleural effusion
- The chest radiograph shows multifocal smooth interlobular septal thickening
- The chest radiograph shows a possible focal air space opacity
- The chest radiograph shows small cavitary pulmonary nodules
Cite as: Larsen BT, Gotway MB. August 2017 imaging case of the month. Southwest J Pulm Crit Care. 2017;15(2):69-79. doi: https://doi.org/10.13175/swjpcc098-17 PDF

Reader Comments