Medical Image of the Week: Spontaneous Pneumomediastinum
 Wednesday, March 30, 2016 at 8:00AM
Wednesday, March 30, 2016 at 8:00AM 
Figure 1. Upright chest radiograph showing pneumomediastinum tracking into neck and small right apical pneumothorax (arrows).
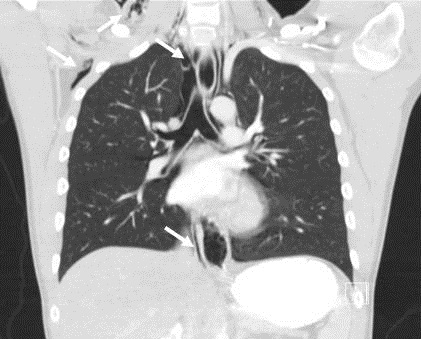
Figure 2. Coronal slice of CT chest showing extensive pneumomediastinum and subcutaneous emphysema (arrows).
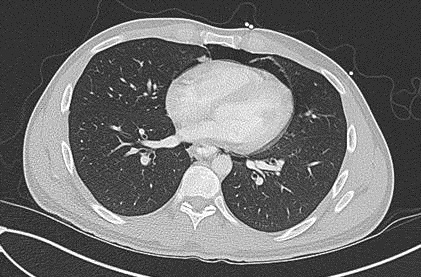
Figure 3. CT scan of chest showing the Macklin effect with air tracking along the bronchovascular sheath in the left lower lobe.
A 24-year-old man with a past medical history significant for type I diabetes mellitus presented to the emergency department with complaints of nausea and vomiting for several days. He reported he had been on drinking alcohol heavily 4 days prior to presentation and subsequently had multiple episodes of vomiting. Initial laboratory evaluation was consistent with diabetic ketoacidosis (DKA). A routine chest x-ray was obtained to evaluate for an infectious etiology of his DKA and revealed pneumomediastinum and a small right apical pneumothorax (Figure 1). A CT scan of the chest was done and showed extensive pneumomediastinum as well as air tracking along the bronchovascular sheaths in the left lower lobe (Figure 2 and 3). It did not reveal evidence of esophageal injury.
Spontaneous pneumomediastinum (SPM) refers to pneumomediastinum that is not associated with noticeable cause such as esophageal rupture or trauma. It is typically a benign condition thought to be due to alveolar rupture and subsequent air tracking along the bronchial tree (1). It has been associated with a number of conditions including asthma, DKA, anorexia nervosa, and other conditions that lead to excessive coughing or vomiting. The radiographic appearance of air dissecting through the pulmonary intersitium along the bronchovascular sheath is known as the Macklin effect and can be seen in Figure 3.
Spontaneous pneumomediastinum typically resolves without complications but must be differentiated from the much more serious diagnosis of esophageal rupture, or Boerrhaave’s syndrome. Boerrhaave’s syndrome is more likely to present with fever, hemodynamic instability, and hydropneumothorax. All patients presenting with suspected SPM should be evaluated for esophageal perforation with a radiographic contrast swallow (2). In our case it was negative for evidence of esophageal disruption and the patient recovered completely.
Lucie Griffin DO and Erik Kraai MD
Division of Pulmonary, Critical Car, and Sleep Medicine
University of New Mexico Health Sciences Center
Albuquerque, NM USA
References
- Murayama S, Gibo S. Spontaneous pneumomediastinum and Macklin effect: Overview and appearance on computed tomography. World J Radiol. 2014 Nov 28;6(11):850-4. [CrossRef] [PubMed]
- Kelly S, Hughes S, Nixon S, Paterson-Brown S. Spontaneous pneumomediastinum (Hamman's syndrome). Surgeon. 2010 Apr;8(2):63-6. [CrossRef] [PubMed]
Cite as: Griffin L, Kraai E. Medical image of the week: spontaneous pneumomediastinum. Southwest J Pulm Crit Care. 2016 Mar;12(3):115-6. doi: http://dx.doi.org/10.13175/swjpcc015-16 PDF

Reader Comments