April 2018 Critical Care Case of the Month
 Monday, April 2, 2018 at 8:00AM
Monday, April 2, 2018 at 8:00AM Clement U. Singarajah, MD
Phoenix VA Medical Center
Phoenix, AZ USA
History of Present Illness
A 70-year-old man was admitted for shortness of breath (SOB) secondary to a “COPD exacerbation/ILD”. A pulmonary consult was placed for possible interstitial lung disease (ILD). A thoracic CT scan for pulmonary embolism showed no embolism and no obvious ILD. He was treated for a COPD exacerbation with the usual therapy of antibiotics, steroids, nebulized bronchodilators and oxygen. He started to improve.
A few days later as he was preparing for discharge, the patient suddenly decompensated becoming more SOB (once more proving that this a dangerous time for patients in hospital). There were reports that this began after he choked and perhaps aspirated on some food and drink. His blood pressure remained stable, but he became tachycardic to 130 beats/min, hypoxic on 100% non-rebreathing mask with saturations of 92%. Obvious clinical acute respiratory failure was present. The patient was started on non-invasive ventilation but continued to deteriorate. He was deemed too unstable to obtain a CT scan. EKG showed sinus tachycardia. The patient was transferred to the ICU for respiratory failure. A chest x-ray was obtained (Figure 1).
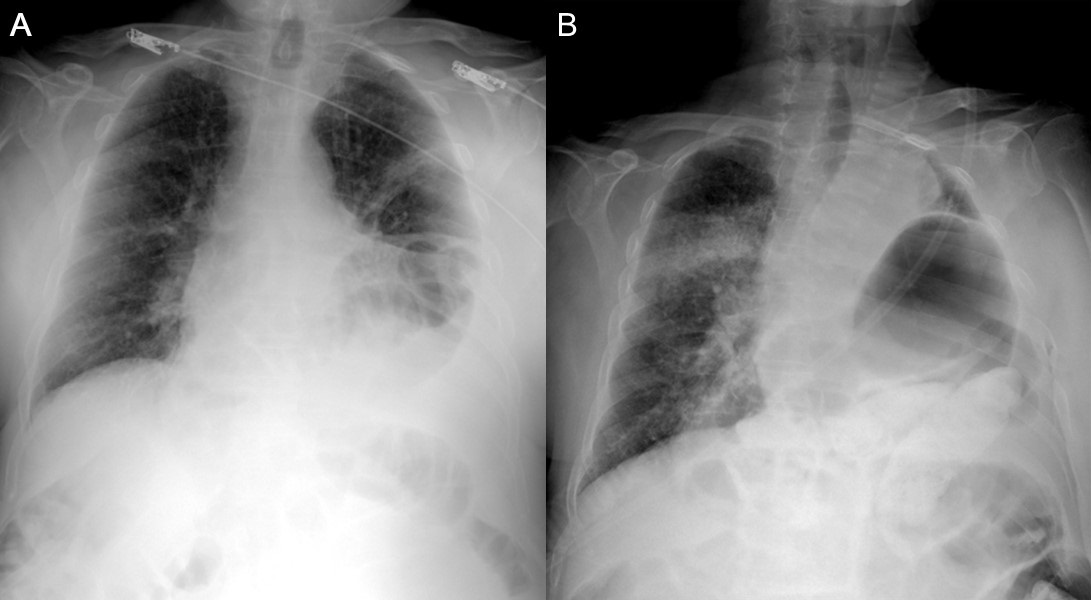
Figure 1. Panel A: Admission chest x-ray which was interpreted as not different from the patient’s previous chest x-ray. Panel B: Portable chest x-ray taken shortly after initiation of non-invasive ventilation just after arrival in the intensive care unit.
The portable chest x-ray taken in the ICU shows a new right-sided consolidation and which of the following? (Click on the correct answer to proceed to the second of six pages)
Cite as: Singarajah CU. April 2018 critical care case of the month. Southwest J Pulm Crit Care. 2018;16(4):183-91. doi: https://doi.org/10.13175/swjpcc042-18 PDF

Reader Comments