March 2016 Critical Care Case of the Month
 Wednesday, March 2, 2016 at 8:00AM
Wednesday, March 2, 2016 at 8:00AM Theo Loftsgard APRN, ACNP
Joel Hammill APRN, CNP
Mayo Clinic Minnesota
Rochester, MN USA
Critical Care Case of the Month CME Information
Members of the Arizona, New Mexico, Colorado and California Thoracic Societies and the Mayo Clinic are able to receive 0.25 AMA PRA Category 1 Credits™ for each case they complete. Completion of an evaluation form is required to receive credit and a link is provided on the last panel of the activity.
0.25 AMA PRA Category 1 Credit(s)™
Estimated time to complete this activity: 0.25 hours
Lead Author(s): Theo Loftsgard APRN, ACNP. All Faculty, CME Planning Committee Members, and the CME Office Reviewers have disclosed that they do not have any relevant financial relationships with commercial interests that would constitute a conflict of interest concerning this CME activity.
Learning Objectives:
As a result of this activity I will be better able to:
- Correctly interpret and identify clinical practices supported by the highest quality available evidence.
- Will be better able to establsh the optimal evaluation leading to a correct diagnosis for patients with pulmonary, critical care and sleep disorders.
- Will improve the translation of the most current clinical information into the delivery of high quality care for patients.
- Will integrate new treatment options in discussing available treatment alternatives for patients with pulmonary, critical care and sleep related disorders.
Learning Format: Case-based, interactive online course, including mandatory assessment questions (number of questions varies by case). Please also read the Technical Requirements.
CME Sponsor: University of Arizona College of Medicine
Current Approval Period: January 1, 2015-December 31, 2016
Financial Support Received: None
History of Present Illness
A 58-year-old man was admitted to the ICU in stable condition after an aortic valve replacement with a mechanical valve.
Past Medical History
He had with past medical history significant for endocarditis, severe aortic regurgitation related to aortic valve perforation, mild to moderate mitral valve regurgitation, atrial fibrillation, depression, hypertension, hyperlipidemia, obesity, and previous cervical spine surgery. As part of his preop workup, he had a cardiac catheterization performed which showed no significant coronary artery disease. Pulmonary function tests showed an FEV1 of 55% predicted and a FEV1/FVC ratio of 65% consistent with moderate obstruction.
Medications
Amiodarone 400 mg bid, digoxin 250 mcg, furosemide 20 mg IV bid, metoprolol 12.5 mg bid. Heparin nomogram since arrival in the ICU.
Physical Examination
He was extubated shortly after arrival in the ICU. Vitals signs were stable. His weight had increased 3 Kg compared to admission. He was awake and alert. Cardiac rhythm was irregular. Lungs had decreased breath sounds. Abdomen was unremarkable.
Laboratory
His admission laboratory is unremarkable and include a creatinine of 1.0 mg/dL, blood urea nitrogen (BUN) of 18 mg/dL, white blood count (WBC) of 7.3 X 109 cells/L, and electrolytes with normal limits.
Radiography
His portable chest x-ray is shown in Figure 1.
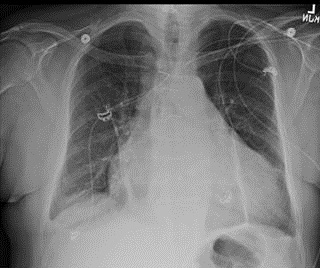
Figure 1. Portable chest x-ray taken on admission to the ICU.
What should be done next? (Click on the correct answer to proceed to the second of five panels)
- Bedside echocardiogram
- Diuresis with a furosemide drip because of his weight gain and cardiomegaly
- Observation
- 1 and 3
- All of the above
Cite as: Loftsgard T, Hammill J. March 2016 critical care case of the month. Southwest J Pulm Crit Care. 2016;12(3):81-8. doi: http://dx.doi.org/10.13175/swjpcc018-16 PDF

Reader Comments