A 45-YEAR-OLD MAN WITH EXCESSIVE DAYTIME SOMNOLENCE, AND WITNESSED APNEA AT ALTITUDE
 Tuesday, April 5, 2011 at 3:32PM
Tuesday, April 5, 2011 at 3:32PM Rebecca Keith MD
University of Colorado Denver, Denver, CO
Carolyn H. Welsh MD
Veterans Affairs Medical Center, Denver, CO
Professor of Medicine
Division of Pulmonary Sciences and Critical Care Medicine, University of Colorado Denver, Denver, CO
Study performed at Denver Veterans Affairs Medical Center
Reference as: Keith R, Welsh CH. A 45-year-old man with excessive daytime somnolence, and witnessed apnea at altitude. Southwest J Pulm Crit Care 2011;2:53-57. (Click here for PDF version)
Abstract
A sleepy man without sleep apnea at 1609m (5280 feet) had disturbed sleep at his home altitude of 3200m (10500 feet). In addition to common disruptors of sleep such as psychophysiologic insomnia, restless leg syndrome, alcohol and excessive caffeine use, central sleep apnea with periodic breathing can be a significant cause of disturbed sleep at altitude. In symptomatic patients living at altitude, a sleep study at their home altitude should be considered to accurately diagnose the presence and magnitude of sleep disordered breathing as sleep studies performed at lower altitudes may miss this diagnosis. Treatments options differ from those to treat obstructive apnea. Supplemental oxygen is considered by many to be first-line therapy.
Case Report
A 45 year old man presents for evaluation of poor sleep, daytime somnolence, and morning headaches. His bed partner reports that he has loud snoring, gasping arousals, and frequent episodes of apnea. He is an obese man with diabetes, hypertension, rhinosinusitis, and gastroesophageal reflux disease who is a long time resident at 3200m (10500 feet). Polysomnography performed at 1609m (5280 feet) showed a normal apnea-hypopnea index (AHI) of 1.4. He spent less than one minute with an oxygen saturation (SaO2) less than 88%.
Given the severity of his symptoms, a home cardiopulmonary sleep study was performed at 3200m (10500 feet). AHI was 39 non-supine and 56 supine. A representative portion of his study is shown in Figure 1. It demonstrates the absence of respiratory effort during apnea events, consistent with central sleep apnea from periodic breathing at altitude.
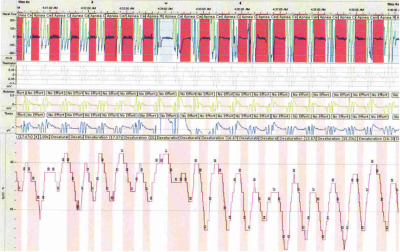
Figure 1. This is a representative example of breathing during sleep. The upper two channels show nasal (nasal flow) and oral air flow (thermistor). Respiratory effort signals in the abdomen and thorax are shown in the next two channels and oxygen saturation in the bottom tracing. A ten minute period of recording is displayed. (Click here for JPEG image)
Discussion
Central apnea is characterized by recurrent episodes of apnea resulting from temporary loss of ventilatory effort. These episodes generally result from a strong dependence on the metabolic control of ventilation during sleep.1 Conditions inducing a reduced partial pressure of carbon dioxide in arterial blood (PaCO2) can precipitate a central apnea, often associated with an arousal and leading to daytime somnolence.
At higher altitudes, the fraction of inspired oxygen (FiO2) is the same as it is at sea level, but the barometric pressure and oxygen tension are less, so the partial pressure of oxygen in arterial blood (PaO2) and SaO2 tend to be reduced. This tendency toward hypoxemia elicits a series of physiologic responses including increased alveolar ventilation, lowering the resting PaCO2, shrinking the gap between the resting PaO2 and the PaCO2 associated with apnea (the apnea threshold). People with sensitive chemoreceptors are more likely to develop periodic breathing at altitude. An increased ventilatory response to hypoxemia may reduce PaCO2 below the apnea threshold. The resultant apnea will eventually result in worsened hypoxemia, which will trigger hyperventilation setting up the oscillating pattern of apnea and hyperventilation typical of periodic breathing.1 Of note, these responses seem primarily related to hypoxemia rather than low barometric pressure as they are present in simulated normobaric hypoxia equivalent to 2000m (6562 feet) altitude .2
Central sleep apnea encompasses multiple disorders including narcotic-induced central apnea, obesity-hypoventilation syndrome, Cheyne-Stokes breathing often seen with heart failure or cerebrovascular disease, and high altitude-induced periodic breathing. Periodic breathing at altitude has the pattern of apneic episodes with cycles of hypoxemia, subsequent hyperventilation, hypocapnia, and resulting apnea described above. The skeletal muscle atonia and reduced respiratory drive3 that normally occurs during rapid eye movement (REM) sleep typically terminates the periodicity by eliminating hyperventilation and restoring regular breathing. Thus, periodic breathing at altitude is seen primarily during non-REM sleep.4 This aberrant respiratory pattern may initially be beneficial at high altitude since the hyperventilation increases SaO2 by 2.9±1.5%, thus improving hypoxemia.4 In our patient, this potential benefit was overcome by a significant increase in sleep disturbance leading to sleep deprivation as well as mental and physical impairment.
Treatment options for periodic breathing at altitude include nighttime oxygen therapy, acetazolamide, and sedative-hypnotics. Supplemental oxygen breaks the apnea cycle by eliminating the hypoxemia that results in hyperventilation, hypocapnia, and apnea. Studies of supplemental oxygen at altitude have shown that subjects spend more time in deep sleep and have improvements in SaO2, tidal volume and AHI.5
Acetazolamide, a carbonic anhydrase inhibitor, induces a metabolic acidosis by urinary elimination of bicarbonate. This is thought to increase ventilation, left-shift the hypercapnic ventilatory response and thus reduce apnea events. Acetazolamide can significantly improve sleep disordered breathing and oxygen saturation during sleep.6 Sedative-hypnotic agents have also improved slow wave sleep at altitude without adversely affecting respiration or performance. This improvement is thought to be secondary to a decrease in wakefulness after sleep onset and improved sleep efficiency.7
This patient presented with classic symptoms of sleep apnea with a negative sleep study at 1609m (5280 feet), arousing clinical suspicion for periodic breathing at altitude. A repeat home sleep study revealed moderate to severe central sleep apnea. After treatment with oxygen and acetazolamide his symptoms significantly improved and repeat home monitoring demonstrated an AHI of 6. Treatment with oxygen alone resulted in improvement as well with an AHI of 13.
Central sleep apnea and periodic breathing are common causes of disturbed sleep at altitude. Symptomatic patients living at altitude should have a sleep study at their home altitude to accurately diagnose the presence and magnitude of sleep disordered breathing. Oxygen is considered by many to be first line therapy.
References
1. Eckert DJ, Jordan AS, Merchia P, Malhotra A. Central sleep apnea: Pathophysiology and Treatment. Chest 2007; 131(2): 595-607.
2. Kinsman TA, Hahn AG, Gore CJ, Wilsmore BR, Martin DT, Chow CM. Respiratory events and periodic breathing in cyclists sleeping at 2,650-m simulated altitude. Journal of Applied Physiology 2002; 92 (5): 2114-8.
3. Schafer, T, Schlafke ME, Respiratory changes associated with rapid eye movements in normo- and hypercapnia during sleep. Journal of Applied Physiology 1998; 85: 2213-2219.
4. Salvaggio A, Insalaco G, Marrone O, et al. Effects of high-altitude periodic breathing on sleep and arterial oxyhaemoglobin saturation. European Respiratory Journal 1998; 12 (2): 408-13.
5. Windsor JS, Rodway GW. Supplemental oxygen and sleep at altitude. High Altitude Medicine & Biology 2006; 7 (4): 307-11.
6. Fischer R, Lang SM, Leitl M, Thiere M, Steiner U, Huber RM. Theophylline and acetazolamide reduce sleep-disordered breathing at high altitude. European Respiratory Journal 2004; 23 (1): 47-52.
7. Beaumont M, Batejat D, Pierard C, et al. Zaleplon and zolpidem objectively alleviate sleep disturbances in mountaineers at a 3,613 meter altitude. Sleep 2007; 30 (11): 1527-33.
Acknowledgments:
Rebecca Keith was the primary author writing the manuscript. Carolyn Welsh also contributed to content and manuscript preparation and revision.
Corresponding author: Rebecca Keith MD
National Jewish Health
1400 Jackson Street
Denver, CO 80206
Phone: 303-398-1511
FAX: 303-398-1381
No financial support was provided for this manuscript and there is no off-label or investigational use of medications or devices.
Dr Keith has no conflict of interest to disclose
Dr. Welsh has no conflict of interest to disclose
Abbreviation List:
AHI - Apnea hypopnea index, the number of apneas or hypopneas per hour of sleep or recording
m – Meters
FiO2 – Fraction of inspired oxygen
PaCO2 - Partial pressure of carbon dioxide in arterial blood
PaO2 – Partial pressure of oxygen in arterial blood
REM – Rapid eye movement
SaO2 – Percentage of available hemoglobin that is saturated with oxygen

Reader Comments