Pulmonary Nocardiosis and Empyema in a Patient with Metastatic Neuroendocrine Tumor
 Saturday, August 13, 2011 at 10:48AM
Saturday, August 13, 2011 at 10:48AM Nimesh K. Patel, DO
Linda Snyder, MD
University of Arizona, Department of Medicine. Tucson, Arizona
Reference as: Patel NK, Snyder L. Pulmonary nocardiosis and empyema in a patient with metastatic neuroendocrine tumor. Southwest J Pulm Crit Care 2011;3:28-33. (Click here for a PDF version)
Abstract
Nocardia is a ubiquitous aerobic gram-positive bacterium that can cause local or disseminated infection. Nocardiosis involves the lung in the majority of cases. Nocardiosis is often an opportunistic infection, but can also affect non-immunocompromised hosts. This case report highlights the presence of empyema due to Nocardia cyriacigeorgica infection, an unusual feature of Nocardia pulmonary involvement.
Case Presentation
History of Present Illness: A 65 year-old male with a history of metastatic neuroendocrine tumor of the pancreas, was admitted to the hospital with a one-week history of hemoptysis, cough, and dyspnea. He was treated for presumed community acquired pneumonia with moxifloxacin two weeks prior to admission. He was receiving monthly octreotide injections for treatment of the neuroendocrine tumor. The patient had no history of corticosteroid use.
Physical examination:
Vital signs: Temperature 99.9F, Respirations18, Blood Pressure 104/69, Pulse 96, SaO2 91% on oxygen at 2 liters per minute by nasal cannula
General: The patient was in no acute distress. He was alert and oriented to person, place and time.
HEENT: No significant abnormalities.
Chest: Dullness to percussion, mid-lower right thoracic cavity, with scattered crackles.
Cardiovascular: regular rate, normal S1 and S2, no murmurs appreciated. Abdomen: positive bowel sounds, soft, non-tender, non-distended, positive hepatosplenomegaly.
Extremities: +2 pitting edema bilaterally extending to mid-thigh level
Laboratory and radiographic findings: The peripheral white blood cell count was 8, 000 cell/mm3 with a differential as follows 91% neutrophils/bands, 7% lymphocytes, 1% myelocyte, 1% reactive lymphocyte, hemoglobin was 11 g/dL and the platelet count was normal. The basic metabolic panel revealed blood urea nitrogen of 30 mg/dl and creatinine of 1.5 mg/dl. The hepatic panel was normal except for an elevated alkaline phosphatase of 530 IU/L. Coccidioides IgM and IgG serology performed by immunodiffusion were negative.
The chest radiographs from two weeks prior to admission (Figure 1), admission (Figure 2) and admission computerized tomography of the chest (Figure 3) are shown.
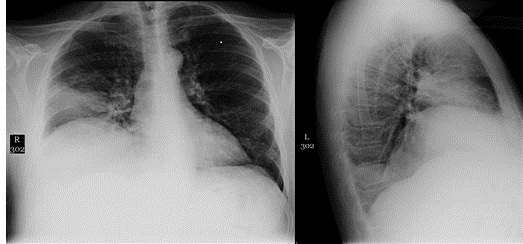
Figure 1. Chest radiograph two weeks before admission: Right middle lobe consolidation with volume loss and small right pleural effusion
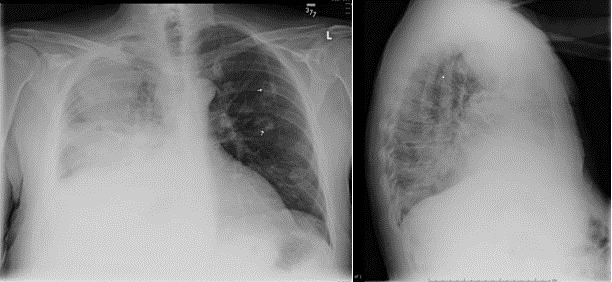
Figure 2. Chest radiograph on admission: Increasing patchy opacifications involving the right upper lobe, right middle lobe, and left lower lobe, with cavity formation noted in the left lung. There is right paratracheal lymphadenopathy noted.
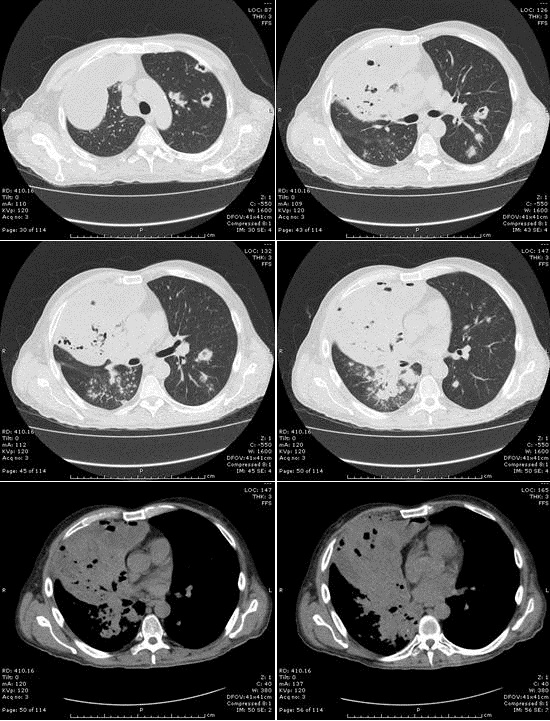
Figure 3: Computerized tomography of the chest showing multifocal consolidation with a necrotizing process containing central lucencies. A loculated, moderate sized right anterior pleural effusion with lucencies is compatible with an empyema.
Hospital course:
Our patient was started on broad-spectrum antimicrobial therapy and underwent chest tube drainage of the loculated effusion. A sputum gram stain revealed 4+ weakly acid-fast branching bacilli, consistent with Nocardia. The gram stain of the pleural fluid showed 3+ polymorphonuclear cells and 3+ gram-positive, branching, weakly acid-fast bacilli, consistent with Nocardia. The culture from sputum and pleural fluid grew Nocardia cyriacigeorgica.
Computerized tomography of the brain showed no intracranial abnormalities. The patient was treated with high dose trimethoprim/sulfamethoxazole, two double strength tablets three times a day with monitoring of sulfamethoxazole levels. The patient clinically improved with antimicrobial treatment and drainage of the empyema. The chest tube was successfully removed and the patient’s symptoms of cough and dyspnea resolved. A chest x-ray showed resolution of the right middle lobe and left lower lobe infiltrative process.
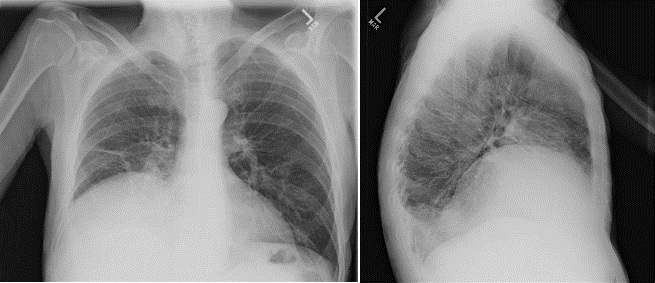
Figure 4. Chest radiograph post-antimicrobial treatment: Interval resolution of right middle lobe and left lower lobe infiltrative process. Post infectious inflammatory changes are noted in the right middle lobe.
Discussion
Nocardiosis is an important opportunistic infection caused by aerobic actinomycetes in the genus Nocardia. Nocardia asteroides has been considered the most common species to cause human disease, however classification has become more complex with the use of molecular techniques. Species formerly included in the Nocardia asteroides complex are now considered distinct species. Nocardia cyriacigeorgica is one of the more common isolates and has been noted to cause pleural disease and empyema. Nocardia species are found in soil and can become airborne; the most common route of entry for infection is inhalation. Effective cell-mediated immunity of the host is crucial to combating infection with Nocardia species. Two recent reviews of nocardiosis highlight important clinical features of this disease (1,2). The most common symptoms are fever, cough, pleuritic chest pain and headache. Specific risk factors for Nocardia infection are present in the majority of patients and include corticosteroid treatment and immunosuppression. Additional risk factors include malignancy and chronic lung disease. Of interest to pulmonologists, chronic obstructive pulmonary disease (COPD) was a common underlying condition, representing over 20% of patients with nocardiosis in these reports. Common chest radiographic presentations of pulmonary nocardiosis include consolidation, nodules and cavities. The diagnosis of pulmonary nocardiosis is made from sputum and bronchoalveolar lavage specimens in the majority of patients. In addition, recent reviews document that pleural effusions are present in up to 35% of patients with pulmonary nocardiosis. In one report, when pleural fluid was sampled, Nocardia was isolated in the majority of patients. Nocardia cyriacigeorgica can cause invasive pulmonary disease and was found to be the predominant species in pulmonary nocardiosis in one review.
Summary
Nocardiosis is an important opportunistic pulmonary disease. The diagnosis should be included in the differential diagnosis of pulmonary infiltrates in immunosuppressed populations, including patients after organ transplantation, with advanced HIV infection and those receiving chronic corticosteroid therapy or chemotherapy. Radiographic findings of lung involvement are variable and include single or multiple nodules or cavities, alveolar or interstitial infiltrates, and pleural effusions. This case report highlights the unusual presentation of Nocardia cyriacigeorgica pulmonary infection with extensive cavitary parenchymal disease and concomitant empyema.
References
- Minero MV, et al. Nocardiosis at the Turn of the Century. Medicine 2009;88:250-61.
- Tomas RM, et al. Pulmonary Nocardiosis: Risk factors and outcomes. Respirology 2007;12:394-400 .
- Latef SM, et al. Nocardia cyriacigeorgica empyema in 45-yr-old male with dual granulomatous lung disease. Chest 2008 134:c12001.
- Schlaberg R. Nocardia cyriacigeorgica: an emerging pathogen in the United States. Journal of Clinical Microbiology 2008;46:265-73.
- Maraki S. Nocardia cyriacigeorgica pleural empyema in an immunocompromised patient. Diagnostic Microbiology and Infectious Disease 2006;56:333-5.

Reader Comments