A 61 Year Old Immunosuppressed Man With A Symptomatic Pulmonary Infiltrate
 Monday, February 14, 2011 at 2:43PM
Monday, February 14, 2011 at 2:43PM Carmen Luraschi-Monjagatta1
Amber Noon1
Neil Ampel1
Suzette Chavez1
Mitch Goldman2
Kenneth S Knox1
University of Arizona, Department of Medicine. Southern Arizona VA Healthcare System. Tucson, Arizona1
Indiana University School of Medicine, Indianapolis, IN2
Reference as: Luraschi-Monjagatta C, Noon A, Ampel N, Chavez S, Goldman M, Knox KS. A 61 year old immunosuppressed man with a symptomatic pulmonary infiltrate. Southwest J Pulm Crit Care 2011;2:17-24. (Click here for PDF version)
Abstract
Coccidioidomycosis is a common cause of community acquired pneumonia in Arizona. Although self-limited in the majority of patients, immunosuppression often causes a blunting of symptoms and a poor antibody response. We present a patient with coccidioidomycosis while receiving adalimumab for psoriasis. The diagnosis was challenging due to negative serology and constellation of symptoms on immunosuppression.
Case Presentation
History of Present Illness
A 61 year-old man with a history of psoriatic arthritis was admitted to the hospital after 5 days of fever, night sweats, dry cough, dyspnea, fatigue and inspiratory chest pain. He was treated for a bacterial community-acquired pneumonia and discharged but was readmitted 2 days later because of persistent symptoms.
On readmission he noted that the fevers had resolved, but stated his other symptoms remained unchanged. Twelve years previously, he had been diagnosed with psoriatic arthritis and was initially treated with methotrexate and prednisone. Due to poorly controlled disease, adalimumab was initiated 6 weeks prior to his illness. Coccidioides serology and tuberculin skin testing were negative at that time.
Physical examination
On re-admission vital signs were within normal limits. Oxygen saturation was 95% on ambient air. He was a well developed man in no acute distress. There was a faint maculopapular rash on his trunk and erythematous plaques with dry silver scale on his limbs. Inspiratory crackles were auscultated over the left lung field anteriorly. Cardiac, abdominal and neurological examinations were normal.
Laboratory findings
The peripheral blood white cell count was 12,200 cell/mm3 with 12.2 % eosinophils. Other laboratory tests, including hematocrit and hemoglobin, platelets, basic metabolic panel and hepatic panel, were normal. Coccidioides IgM and IgG serology performed by immunodiffusion were negative. The re-admission chest radiography (Figure 1) and computed tomography of the chest (figure 2) are shown.
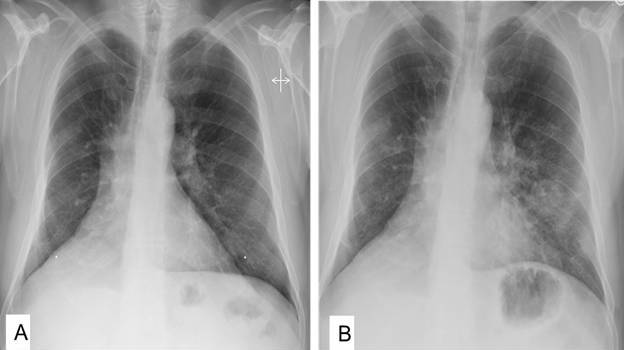
Figure 1: A: Pulmonary radiograph two months before admission. B: Pulmonary radiograph at admission.

Figure 2: Computerized tomography of the chest showing left lower lobe lesions, left hilar adenopathy, and a right pulmonary nodule (arrow).
A left-sided pulmonary parenchymal infiltrate, already observed during the first admission, with left hilar adenopathy, were the predominant findings. Indistinct right sided densities were newly appreciated. Bronchoscopy with bronchoalveolar lavage (BAL) was performed which showed a normal airway and a cell differential of 18% macrophages, 14% neutrophils, 15% lymphocytes and 53% eosinophils. A Papanicolau stain was negative for fungal elements. Culture of the BAL fluid was obtained.
Hospital course
Our patient remained stable with persistent symptoms during his brief hospital stay. Antibacterial treatment for community acquired pneumonia was discontinued and the patient was sent home. Three days later cultures grew Coccidioides. The patient was referred to the Valley Fever Center and started on fluconazole with near complete resolution of his symptoms. Therapy for psoriasis was not restarted. After 4 weeks, the immunodiffusion (IDTP) turned positive at a titer of 1:4.
Discussion
Coccidioidomycosis is a soil-borne fungal infection encountered predominantly in the southwestern United Stated and northern Mexico. In the United States, 60% of symptomatic cases are currently reported from Arizona. Two species, Coccidioides immitis and C. posadasii, are the causative agents. Three important points are illustrated by this case. First, coccidioidomycosis can often be mistaken for a bacterial community acquired pneumonia. Second, the diagnosis of coccidioidomycosis can be challenging, with serology sometimes negative in patients with underlying immunosuppression. Third, therapy with inhibitors of TNF-α may increase the risk of symptomatic coccidioidomycosis.
Among populations living in the endemic coccidioidal region, approximately 25% of patients presenting to urgent care clinics with community-acquired pneumonia have coccidioidomycosis.(1) The diagnosis can be difficult, but the presence of erythema nodosum, hilar or mediastinal lymphadenopathy on chest radiograph, and peripheral blood eosinophilia are suggestive of coccidioidomycosis.
Serologic tests for coccidioidomycosis may take up to six weeks in immunocompetent individuals to become positive. Several different assays for coccidioidal antibodies are currently available (2). Acute IgM reactions can be detected using the tube precipitin (TP) assay, immunodiffusion (IDTP), or enzyme immunoassay (EIA). For detection of IgG, complement fixation (CF), immunodiffusion (IDCF), or EIA can be employed. The CF and IDCF can be titrated and elevated titers are an indication of more severe disease.
Serologic assays for coccidioidomycosis are very specific. Serology testing for coccidioidomycosis is routinely and repeatedly performed during an acute infection but can take up to six weeks in immunocompetent individuals to produce reliably detectable antibodies. In acute disease, IgM can be detected with serologic tests in up to 53% of patients in the first week, which increases to 75% in the presence of erythema nodosum and further increases to 91% at 3-4 weeks of infection (3). However, in the immunosuppressed patient these tests are less likely to be positive than among immunocompetent patients. Coccidioides antigen testing may be useful in patients with large fungal burden (4). In our patient, serology was initially negative, but eventually became positive.
When suspecting pulmonary coccidioidomycosis, a bronchoscopy with bronchoalveolar lavage (BAL) is often performed. Cell differentials frequently show a high percentage of eosinophils. Blood and BAL eosinophilia is common in Coccidioidomycosis. In several recent cases, we have seen intense eosinophilic pneumonia (>50% eosinophils in BAL) due to Coccidioides infection. Although it is tempting to diagnose acute eosinophilic pneumonia in these instances, it is important to keep Coccidioides infection in the differential diagnosis, especially in endemic areas. Cytology examination of BAL secretions can give a rapid diagnosis, but the sensitivity is low, even in severely immunocompromised patients. The Papanicolaou stain is superior to other stains in identifying Coccidioides spherules when compared with 10% potassium hydroxide and to calcofluor white staining. Culture of bronchial specimens increases the yield. The gold standard for the diagnosis of coccidiodomycosis is culture or visualization of spherules in tissue. Coccidioides grows on routine bacterial or fungal media in three to seven days at 35°C. Growth of Coccidioides on solid culture media is a major hazard for infection and microbiology laboratories should always be alerted when coccidioidomycosis is suspected. In our case, Coccidioides grew from BAL fluid, confirming the diagnosis.
In humans, an effective response to coccidioidal infection depends on an intact cellular immune response. In this regard, an increased risk of symptomatic coccidioidomycosis (both reactivation and newly acquired infection) in patients with inflammatory arthritis receiving TNF-α antagonists has been documented (5,6). Primary anti-fungal prophylaxis for patients in the endemic area starting anti-TNF therapy is not recommended, but adequate data regarding this subject is lacking. In our practice we check coccidioidomycosis serology and a CXR prior to initiation of anti-TNF therapy and then annually. Although the timing of discontinuing adalimumab in our patient might raise suspicion for immune reconstitution inflammatory syndrome (IRIS), to date Coccidioides related IRIS has not been definitively reported upon withdrawal of anti-TNF therapy.
Summary
Coccidioidomycosis is a common cause of community acquired pneumonia in the endemic area. The diagnosis should be included in the differential diagnosis of pulmonary infiltrates with eosinophilia. Immunosuppression with anti TNF- α therapy increases the risk for a negative serologic response in coccidioidomycosis.
References
- Valdivia L, Nix D, Wright M, Lindberg E, Fagan T, Lieberman D, Stoffer T, Ampel NM, Galgiani JN. Coccidioidomycosis as a common cause of community-acquired pneumonia. Emerg Infect Dis 2006;12:958-62.
- Blair JE, Coakley B, Santelli AC, Hentz JG, Wengenack NL. Serologic testing for symptomatic coccidioidomycosis in immunocompetent and immunosuppressed hosts. Mycopathologia 2006; 162:317-24.
- Smith CE, Saito MT, Simons SA. Pattern of 39,500 serologic tests in coccidioidomycosis. JAMA. 1956;160:546-52
- Durkin M, Estok L, Hospenthal D, Crum-Cianflone N, Swartzentruber S, Hackett E, Wheat LJ. Detection of Coccidioides antigenemia following dissociation of immune complexes. Clin Vaccine Immunol. 2009;16(10):1453-6.
- Bergstrom L, Yocum DE, Ampel NM, Villanueva I, Lisse J, Gluck O, Tesser J, Posever J, Miller M, Araujo J, Kageyama DM, Berry M, Karl L, Yung CM. Increased risk of coccidioidomycosis in patients treated with tumor necrosis factor alpha antagonists. Arthritis Rheum 2004; 50:1959-66.
- Ampel NM. New perspectives in coccidioidomycosis. Proc Am Thorac Soc 2010: 7: 181-5.
Corresponding author:
Kenneth S Knox, M.D.
Associate Professor of Medicine, University of Arizona
Southern Arizona VA Health Care System
3601 S 6th Ave (1-11C)
Tucson, AZ 85723
Tel: 520-629-1848 Fax: (520) 629-4976
Acknowledgment:
We would like to thank the Valley Fever Center for Excellence http://www.vfce.arizona.edu/ for its support
Author Contributions:
- Drs. Luraschi-Monjagatta and Knox had full access to data in the report and take full responsibility for the integrity and the accuracy of the report.
- Report concept and design: Drs. Luraschi-Monjagatta and Knox.
- Acquisition of data: Drs. Luraschi-Monjagatta, Noon, Knox and Ms Chavez.
- Drafting of the manuscript: Dr. Luraschi-Monjagatta, Ampel and Knox.
- Critical revision of the manuscript for important intellectual content: Drs. Goldman, Ampel, and Knox.
Abbreviations:
tube precipitin (TP), immunodiffusion tube precipitin (IDTP), enzyme immunoassay (EIA), complement fixation (CF), immunodiffusion compliment fixation (IDCF), Bronchoalveolar lavage (BAL), Immune reconstitution inflammatory syndrome (IRIS)

Reader Comments