A Case of Mislabeled Identity
 Thursday, December 30, 2010 at 12:53PM
Thursday, December 30, 2010 at 12:53PM Reference as: Singarajah C, Park K. A case of mislabeled identity. Southwest J Pulm Crit Care 2010;1:22-27. (Click here for PDF version)
A 60-year-old man in the surgical intensive care unit for atrial fibrillation with rapid ventricular response, on his second post-operative day following colectomy, complained of worsening shortness of breath. A chest radiograph (Figure 1) was obtained. A chest radiograph performed one day previous to Figure 1 showed clear lungs, no pleural effusions, and no volume loss.
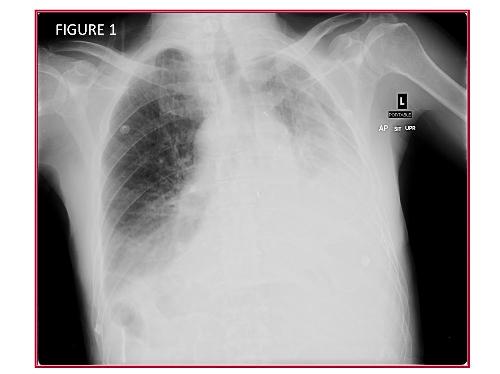
Question 1 and Figure 1: What are the abnormal findings on the chest radiograph? In particular, what technical error has occurred?
The frontal chest radiograph shows increased opacity in the bases bilaterally, greater on the side labeled left (see “L” in the image- this is the technologist’s marker). Note the shift of the trachea towards the side labeled left. However, note also the opacity along the superior mediastinum on the right side; this opacity has the appearance of the aortic arch. Note the appearance of the stomach below the diaphragm, ipsilateral to the aortic arch. Also, the opacity at the left lung base shows a configuration resembling the heart. Taken together, these findings raise the possibility that the radiograph is mislabeled, with the “Left” marker (“L”, Figure 1) improperly placed on the patient’s right side. Prior chest radiographs not shown) confirm the patient did not have situs inversus.
There is evidence of volume loss in the right thorax (labeled incorrectly as left in this image). Note the shift of the trachea towards the side with increased lung opacity. The entire left right thorax (again, incorrectly labeled left in this image) is small, and the air column in the right mainstem bronchus abruptly terminated, suggesting endobronchial obstruction.
Furthermore, the patient had no clinical reasons for a new large pleural effusion, and recent prior films showed no pleural fluid.
Surgery was consulted and a procedure was performed. The results of this procedure are shown in Figure 2.

Question 2: What procedure was performed by the surgery team?
The surgery team improperly placed a thoracostomy tube in the left thorax because they misinterpreted Figure 1 as showing a large left pleural effusion. Figure 2 shows the tip of the thoracostomy tube in the medial superior left thorax, associated with subcutaneous emphysema. Progressive volume loss is seen on the right side, again suggesting endobronchial obstruction- note that the residual air in the right upper thorax in Figure 1 is no longer present in Figure 2. The surgery team then improperly placed a thoracostomy tube on the right side, mistaking the small, opacified right thorax for pleural effusion on that side. Figure 3 shows the new right thoracostomy tube tip located over the cranial right thorax.
The surgical team was concerned that the thoracostomy tube showed little fluid output and a second thoracotomy tube was placed on the contralateral side (Figure 3).

This tube also did not show significant output. The pulmonary / critical care medicine team was then consulted. The pulmonary / critical care medicine physician performed a procedure which partially corrected the cause of the patient’s original complaints. The chest radiograph following this procedure is shown in Figure 4.
Question 3: What procedure (s) was performed by the pulmonary / critical care medicine team?
Bronchoscopy was performed, and showed significant mucous plugging. The mucous plugs were removed resulting in improved right lung aeration (Figure 4).

Learning Points:
- Physical exam would have identified improperly labeled chest radiograph
- The chest radiograph shows volume loss, suggesting endobronchial obstruction due to mucous plugging- the side of the thorax showing increased attenuation shows reduced volume. In contrast, pleural effusion would show increased opacity associated with mass effect and shift of the cardiomediastinal structures away from the side of the thorax showing increased attenuation
- Time-outs are no substitute for clinical skills.The patient had two thoracostomy tubes, both placed for incorrect reasons, one of which was placed on the wrong side all together.
- Therapy for atelectasis and mucous plugging includes the following:
- Patient mobilization, ambulation, sitting up;
- Minimize anti-tussive meds (narcotics, etc), minimizes sedation;
- Chest physiotherapy for the affected lung;
- Continuous lateral rotation therapy for patients with altered mental status who cannot mobilize (for example, a Triadyne bed made by KCI or manual turning);
- Bronchoscopy, and;
- Mucolytics are of equivocal benefit
Clement Singarajah MD. Associate Chief Pulmonary and Critical Care Fellowship, Phoenix VA Hospital and Good Samaritan Regional Medical Center, Phoenix AZ.
Kevin Park, MD, Pulmonary and Critical Care Medicine fellow, Phoenix VA Hospital and Good Samaritan Regional Medical Center, Phoenix AZ.

Reader Comments